Those of us with bipolar disorder can bear a heavy burden when it comes to co-occurring conditions, medication side effects, and we are at higher risk for many diseases. Some of these effects are ameliorated by efforts at early screening and detection. We hope (perhaps naively) to catch tardive dyskinesia before it becomes permanent and Stevens-Johnson Syndrome before it becomes fatal. Likewise, in the US we have a federal registry for clozapine patients that aims to detect agranulocytosis (destruction of white blood cells, which disables the immune system) with rigorous blood testing.
Other medications may take a more nefarious route to affecting our health. Lithium is able to cross membranes and take up residence inside your body’s cells, where it stubbornly resists removal by hemodialysis. Years down the road, it can lead to kidney failure, not to mention destroying your thyroid gland.
But there’s more than meets the eye to the interface of bipolar disorder in medical care.
Bipolar disorder is widely stigmatized by medical professionals
I once presented at the ER for an abscess the size of a tennis ball erupting from my thigh (a consequence of my then-undiagnosed hidradenitis). I showed the triage nurse; she documented it. Then she asked for my phone and my shoes.
“The psychiatrist is going to see you,” an aide informed me.
“What? Why? I have an abscess!”
They didn’t care to listen to me. Two hours later, a psychiatry resident showed up at my bedside. He took a look at my abscess.
“I don’t know why they sent you over here,” he said, sighing. Another two hours passed before a “medical” MD came to take a look and determine (within minutes) that we were going to drain my abscess. It was extremely painful. Surely, anyone would be a touch irritable or agitated in such circumstances. But I’ve been told that having bipolar disorder in my history was good enough reason to detain me, independent of any other facts. You know what that’s called: discrimination. I hadn’t complained of any suicidal planning or expressed a desire to be admitted. In my place, someone without those two words in their file — “bipolar disorder” — would have been seen by a medicine doctor hours earlier.
But, to be fair, it’s not just bipolar disorder that is stigmatized. I was once being detained in the psych area of the ER, when an aide mentioned to another aide that she had PTSD. I was in a fairly good mood, and I joked, “You’re one of us!”
“I’m nothing like you,” she said, frowning coldly. “PTSD is not a mental illness.”
I was taken aback by her confidence and we started to argue when the charge nurse walked in. We both told our side of the story and the charge nurse decided to move the aide to a different part of the ER. She did not look happy, let me tell you.
Bipolar disorder can affect how drugs work in your body
Whether from drug-drug interactions or simply unusual metabolism of certain medications, prescribing medicine for physical health reasons is a tricky business when you have bipolar disorder. The most commonplace medications can be problematic: antibiotics (can cause mania), ibuprofen or most other NSAIDs (interacts with lithium and can raise lithium levels to toxic, resulting in profuse vomiting — try telling that to an overworked nurse who thinks you’re seeking pain meds!), prednisone or other steroids (can cause mania), Sudafed (stimulant — may cause mania)… the list goes on.
This is what I’ve found with alternatives. This only represents my own experience and should not be taken as an endorsement of research in this area (probably because there isn’t much).
Antibiotics: Doxycycline should be avoided, but amoxicillin is okay.
Ibuprofen/NSAIDs: The exception to this rule is old-fashioned aspirin, which is safe if you’re on lithium!
Prednisone/steroids: Unfortunately I haven’t found an effective alternative. You just gotta play the odds. Being manic is better than being dead.
Sudafed: I recommend diphenhydramine (Benadryl) which is effective, safe for bipolar disorder, and cheap.
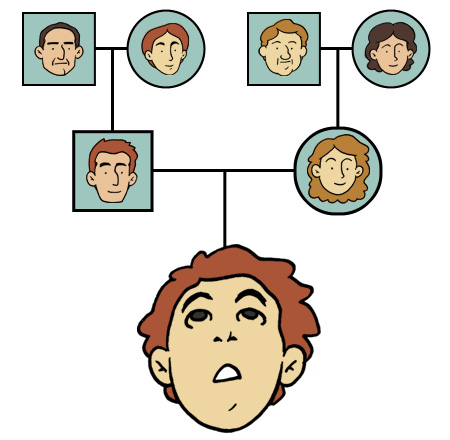
Having bipolar disorder can increase your odds of having another disease
Some diseases and risk factors for diseases, including metabolic syndrome, obesity, diabetes mellitus (type 2), and diabetes inspidus (if you’re on lithium) appear to clearly be linked to certain medications people might take to treat their bipolar disorder. But others are less clear. Headaches are associated with bipolar disorder, especially migraines and cluster headaches (less commonly chronic tension headaches). Genetic evidence has aligned to connect epilepsy and bipolar disorder (such as the SP4 gene, which was published about in September 2024) and this is concordant with the longstanding clinical observation that bipolar disorder often responds to cocktails including anticonvulsant medications such as Lamictal (lamotrigine), Depakote (valproate), even Topamax (topiramate). Large studies have also shown that people with bipolar disorder are more likely to develop Parkinson’s Disease, independently of cases that are likely drug-induced.
Surprisingly, when COVID-19 first swept the world, some research suggested that people with bipolar disorder were more likely to have a severe or life-threatening COVID-19 disease course even when controlling for factors such as obesity. Taken together with available evidence, this may lend support to the idea that alterations in the body’s inflammatory pathways may be causal to bipolar disorder. It has long been recognized that influenza infection can precipitate manic or psychotic episodes. In January 2018 I had the flu and I became preoccupied with the fact that I (definitely) had AIDS and I began writing long goodbye letters to my friends. Luckily, the flu was better in about 3 days.
Drugs (use, abuse, and misuse) cause problems
As I mentioned, certain medications can have severe side effects…
Neuroleptics (such as Haldol/haloperidol): Neuroleptic Malignant Syndrome, Tardive Dyskinesia, Movement Disorder
Atypical Antipsychotics (such as Zyprexa/olanzapine, Risperdal/risperidone, Abilify/aripiprazole, and clozapine): Agranulocytosis (Clozapine specifically); Akathisia and movement disorder (particularly Abilify and Vraylar)
Anticonvulsants: Stevens-Johnson Syndrome (especially lamotrigine — and keep in mind that risk for SJS increases whenever you start or stop taking the medication suddenly, and if you do this multiple times your risk climbs higher and higher)
Antidepressants and other serotonergic drugs, such as stimulants and street drugs like MDMA: Serotonin Syndrome
Bipolar people are famous for resisting taking medications that could help them, which can make the above side effects more likely. Not taking your meds can also make bipolar disorder worse, and make you more at risk for accidental deaths such as a car crash, while also making you more at risk for intentional death (suicide). Lithium has uniquely shown a capacity to lower the risk of suicide.
Not only that, but it will always be assumed that you are “drug seeking” especially when you try to explain the bit about why you’re too good for the ibuprofen that everyone else takes. But no fear, the nurse has your back and will get you some IV lorazepam (Ativan) while they process your discharge.